T: 01822 851370 E: [email protected]
Visit RSN Survey about life in rural England to find out more.
May Edition of Casebook from the Rural Health and Care Alliance
May 2021 Edition
In casebook this month - a significant focus on lock down and the impact of covid on mental health and an exciting foretaste of the launch of a new rural community of practice planned in partnership with the NHS Confed.
NEWS COMMENTARY
Covid: Indian variant could disrupt 21 June easing, PM says
I think there is no doubt that rural places will be adversely affected if we cant push on with the re-opening of the country. However it also seems to me that we are on a knife edge here. This story tells us:
The Indian virus variant could pose "serious disruption" to lockdown easing in England on 21 June, the PM says.
Boris Johnson said if it was found to be "significantly" more transmissible there could be "some hard choices".
The wait between jabs will be cut from 12 weeks to eight for the over-50s and clinically vulnerable because of concern over the variant, he added.
Cases of the Indian coronavirus variant have nearly tripled in the past week, Public Health England figures show.
Surge testing is already taking place in 15 areas across England, including Bolton, Blackburn, London, Sefton and Nottingham.
According to Friday's government figures, a further 17 people have died in the UK within 28 days of a positive test and another 2,193 coronavirus cases have been recorded.
Speaking at a Downing Street briefing alongside the UK's chief medical adviser, Prof Chris Whitty, Mr Johnson said first Covid vaccine doses will also be prioritised "for anyone eligible who has not yet come forward". Currently, England's vaccination rollout is open to people over the age of 38.
The prime minister said he did not believe that the "present evidence" showed a need to delay the next stage in the easing of lockdown in England on Monday - when pubs and restaurants will be allowed to serve customers indoors and six people or two households can meet in a private home.
Full article: https://www.bbc.co.uk/news/uk-57122817
Mental Health Poor for 11 Percent of U.K. Adults During COVID-19
We’re starting to get a significant handle on the impact of Covid in relation to mental health and this story along with the other mental health feature in casebook is very revealing. Its just a shame it doesn’t apply a rural filter to the analysis.
About 11 percent of U.K. adults experienced deteriorating or consistently poor mental health during the COVID-19 pandemic, according to a study published online May 6 in The Lancet Psychiatry.
Matthias Pierce, Ph.D., from the University of Manchester and colleagues tracked average mental health during the pandemic, characterized distinct mental health trajectories, and identified predictors of deterioration. The 12-item General Health Questionnaire was used to assess mental health in 19,763 adults.
The researchers observed a deterioration in average population mental health with onset of the pandemic, which did not begin improving until July 2020. Five distinct mental health trajectories were identified up to October 2020. Most participants had consistently good or very good mental health (39.3 and 37.5 percent, respectively).
Twelve percent comprised a recovery group, who initially experienced a decline in mental health followed by improvement to prepandemic levels by October. For 7.0 percent, there was a steady deterioration in mental health during the pandemic, and for 4.1 percent, mental health declined initially and remained very poor throughout.
The likelihood of having pre-existing mental or physical ill health, living in deprived neighborhoods, and being non-White was increased for these two groups. Subsequent deterioration in mental health was predicted by severe acute respiratory syndrome coronavirus-2 infection, local lockdown, and financial difficulties.
Full article: https://consumer.healthday.com/poor-mental-health-for-11-percent-of-u-k-adults-during-covid-19-2652927675.html
Covid: Will UK vaccine success keep virus at bay?
I suspect, even though I have little evidence to substantiate it, that smaller rural settlements, will be less susceptible to the re-emergence of the pandemic to the same degree as larger urban settings, what do you think? This story tells us:
Next week will see the most significant lifting of restrictions yet in England, with indoor mixing to be allowed. The rest of the UK is making similar steps.
It means the onus is increasingly shifting on to the vaccines, rather than social distancing and restrictions, to keep the virus at bay. How well do they work? And is there now enough immunity in the population to protect us all?
The UK has benefited from both fast rollout and good uptake. Currently, a third of the adult population is fully vaccinated, with another third having had one dose.
Among those at most risk - the over-50s and younger adults with health conditions, where 99% of Covid deaths have occurred - uptake for the first dose has been 95%.
Some describe that as being only partially vaccinated. But that can underplay the significance of that first dose, which provides most of the protection - the second acts to boost immunity and is important for long-lasting protection.
The latest government data - based on evidence from the rollout - suggests one dose of the Pfizer-BioNTech or Oxford-AstraZeneca vaccine cuts the risk of infection by as much as 70% and death by even more.
Data on their effectiveness after two doses is only just emerging - but, as expected, it suggests this level of protection is boosted even further. For Pfizer, which was rolled out first, the risk of death is reduced by 97%.
What is more, those that are vaccinated but do become infected are thought to be about half as likely to pass the virus on.
The vaccines are working about as well as could be hoped in the real world - and confirm what the trial results always suggested.
Full article: https://www.bbc.co.uk/news/health-57073312
Could digital platforms help bolster UK workers' mental health?
The second of our mental health stories adding more flesh to the bones of the clear impact of the pandemic and crying out for the application of a rural lens to measure the specifics of the impact.
UK workers are facing a rise in mental health issues in the wake of the coronavirus pandemic, according to a study by Kooth PLC, a digital mental health and well-being platform.
The Kooth Pulse 2021 report shows lead indicators for mental health in the UK are deteriorating as the nation prepares to leave COVID-19 behind. The research, based on anonymous data from 192,000 people on Kooth’s mental health platforms, covers March 2020 to March of this year.
Among the findings: 17% of adults who sought professional intervention said they think about hurting themselves or feel suicidal nearly every day, a 40% increase over the previous year. Another 41% say that they feel nervous every day.
The data echoes similar findings over the past year, including a report from Slack that found 56% of UK employees experienced burnout in 2020. And research by tech recruitment firm Harvey Nash highlighted a 75% increase in tech workers concerned about their mental health.
Full article: https://www.computerworld.com/article/3618429/could-digital-platforms-help-bolster-uk-workers-mental-health.html
Councils in England facing funding gaps plan to cut special needs support
Many of the most significantly affected authorities and therefore communities referenced here are rural. This story tells us:
Councils in England, facing a funding shortfall of more than half a billion pounds for educating children with special needs, are planning spending cuts and service reviews, according to figures compiled by the Observer.
Campaigners fear children could lose some of their support as local authorities try to clear yawning historical deficits, with government rules stopping them using other reserves to help to fund the special educational needs and disabilities (Send) system.
Figures covering 131 of England’s 151 “upper tier” local authorities show the combined forecast “overspend” on high needs budgets comes to £503m for the 2020-21 financial year.
The figures were obtained from freedom of information requests and council documents, and show forecasts made late in the financial year.
Surrey council confirmed it overspent its high needs budget by £35m in 2020-21, and is forecasting a further overspend of £24m in 2021-22. Kent forecast an overspend of £35.8m in 2020-21, and 14 other councils forecast overspends of £10m to £18m.
Cambridgeshire has a forecast deficit of £13.7m in 2020-21. It is planning to reduce top-up funding for Send children in mainstream schools, as well as launching a variety of reviews covering individual support packages. A council spokesperson said: “In addition to the continuing rise in the number of education, health and care plans (EHCPs) being allocated to those in need, we are seeing an increase in the complexity of need among our children and young people. Our funding allocation is not sufficient to adequately match the increase in demand.”
Full article: https://www.theguardian.com/education/2021/may/15/councils-in-england-facing-funding-gaps-plan-to-cut-special-needs-support
MEMBER ARTICLES
We’d love to hear from you - share what you’re proud of
We have four great articles from members this month, see below. If you have something, you would like us to feature in a future edition, please let us know by clicking here to send us an email.
Mountain Medicine Phd OpportunityApplicants are invited for a PhD studentship in the National Centre for Remote and Rural Medicine within the Faculty of Clinical and Biomedical Sciences. The studentship is tenable for 3 years full time (subject to satisfactory progress). Both Home/EU and International applicants may apply. The studentship will provide an annual stipend of £15,285 (subject to satisfactory progress) in addition to course fees. It is expected that the successful applicant will commence on 1st September 2021.
Project Title: Can global consensus be arrived at as to the essential components of training for ensuring confident and effective medical practice in remote settings?
Project Description:
This project will undertake an initial review of all global programs which seek to train remote medical practitioners. The initial review will inform the first stage of a Delphi process calling on the expertise of leaders in this area from around the world. On completion of the full Delphi process it is hoped to arrive at a draft consensus position for the essential features for training for those practicing in remote locations anywhere in the world.
Click here for further information and how to apply.
Lincolnshire Refugee Doctors Project The numbers of Doctors has increased from 12 to 23, with the project having also been expanded to Lincoln as well as the original location of Grimsby. The programme over the last few months has successfully recruited both social mentor volunteers and English Language volunteers who are actively supporting programme members. Read more
The numbers of Doctors has increased from 12 to 23, with the project having also been expanded to Lincoln as well as the original location of Grimsby. The programme over the last few months has successfully recruited both social mentor volunteers and English Language volunteers who are actively supporting programme members. Read more
Throughout the COVID period 9 of our Doctors have actively supported local hospitals by carrying out Medical Support Worker roles which has helped support the NHS through what has been a hugely challenging period. The Doctors who have carried out these roles have also benefitted hugely by having the opportunity to work in a key role in under supervision whilst on our programme.
The project has been granted some further funding which will be used to support Doctors on the programme with further English Language support from a teacher who will be recruited to join the programme.
As we move into the next of our project, we’d be delighted to hear from Refugee Doctors or Asylum Seeking Doctors who need support, and also anyone who is interested in volunteering to support us.
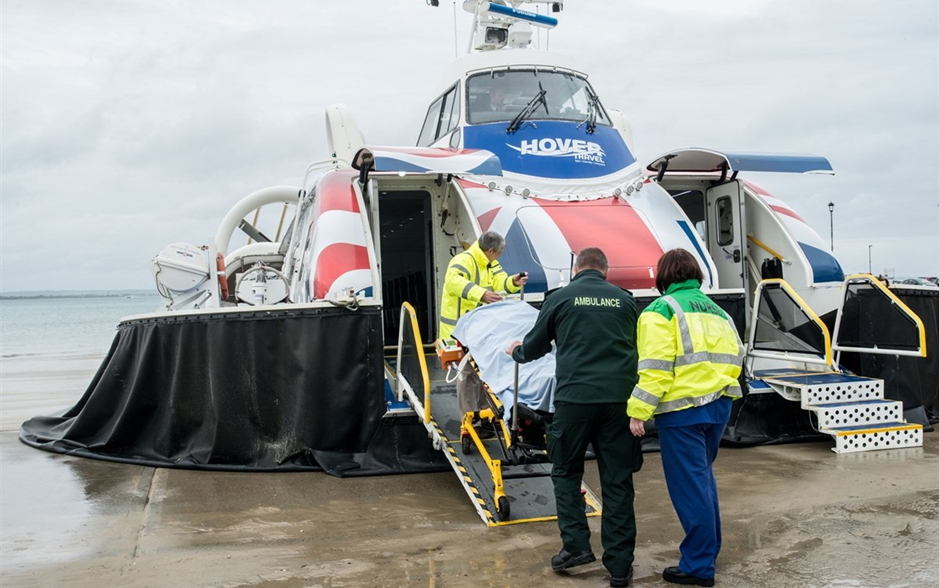
NHS services celebrate partnership with Hovertravel for the benefit of the Isle of Wight residents
The Isle of Wight NHS Trust and a local Island Company Hovertravel have celebrated a partnership which has contributed significantly to the local community. Working closely with the NHS they have developed the Island Rescue service which allows transfers of patients from the Isle of Wight to hospitals in Portsmouth or Southampton significantly reducing transfer times.
Pre covid-19 stretcher patient transfers had been taken in ambulance via the car ferry, a return journey of 4- 6 hours. Following trials with Hovertravel, and working with the South Central Ambulance service, it was established that Hovertravel’s Island Rescue service would provide the quickest option for stretcher patient transfer during the initial lockdown.
The short crossing time meant the ambulance crew are off-island for a much shorter time, as the organised patient handover to the South Central Ambulance Service at Hovertravel’s pad in Southsea means the IOW NHS Trust Ambulance Crew can make an immediate return trip to the island. Over four hours per crossing are saved and this means the ambulance crew are once again available to help patients on the Island.
Recent events have shown how companies can work together for the good of the community and the innovative partnership between Hovertravel and the NHS to transfer stretcher patients across the Solent, whilst conceived during lockdown continues today, with almost 200 patients flown since March.”
To demonstrate the partnership Hovertravel have incorporated both the NHS logo and ambulance logo into their livery.
Neil Chapman, managing director of Hovertravel, said: “Hovertravel is a unique business and our craft are photographed by travellers and onlookers every day. We wanted to celebrate the partnership with two similarly iconic British heritage brands by including their logos in our livery.
Maggie Oldham, Chief Executive at Isle of Wight NHS Trust, said:
“Our partnerships make us stronger and everyone at Isle of Wight NHS Trust is grateful to Hovertravel for its support during our response to COVID-19.
“It has been fantastic to see how our community has come together to meet the challenges of the last few months and the new livery is a powerful demonstration of how organisations can work together.”
Dispensing Doctors’ Association – Local Pharmaceutical Needs Assessment
Health and wellbeing boards (HWBs) in England find themselves with an extra six months in which to prepare their local pharmaceutical needs assessment (PNA) – a process that allows local health and wellbeing service coordinators to reconsider the adequacy of their pharmacy network in light of changes to the local demography.
In view of COVID-19, the deadline for producing the 2021 PNA has now been extended to October, with a view to introduction from April 2022.
For dispensing practices – GPs that dispense medicines in rural locations where pharmacies are not viable – PNAs are important documents because they set out in black and white the areas in which a dispensing practice can actually operate (officially known as a ‘controlled locality’) and they acknowledge the services that a dispensing practice offers - albeit that when assessing the need for a new pharmacy that may replace a GP dispensing service, this aspect of the PNA does not carry as much weight in England as it does in Wales. Read more
Since their introduction in England in 2015 (and in Wales in 2022), PNAs have brought some much-needed stability to the pharmacy/dispensing GP network, even though provisions to allow pharmacies that offer ‘unforeseen benefits’ have continued to exert downward pressure on the dispensing GP network in England. In 2019-20, such applications were the most commonly-used in controlled areas where dispensing GPs operate – accounting for eight of the nine pharmacy applications in these areas.
However, as English authorities tussle with their pharmacy network planning, they may benefit from pausing to consider the effect on their planning of online pharmacies. Due to their operation in a virtual rather than terrestrial neighbourhood – and limitations on the services they offer - online pharmacies fall outside the jurisdiction of the PNA and, thus, effectively drive a coach and horses through the PNA planning process.
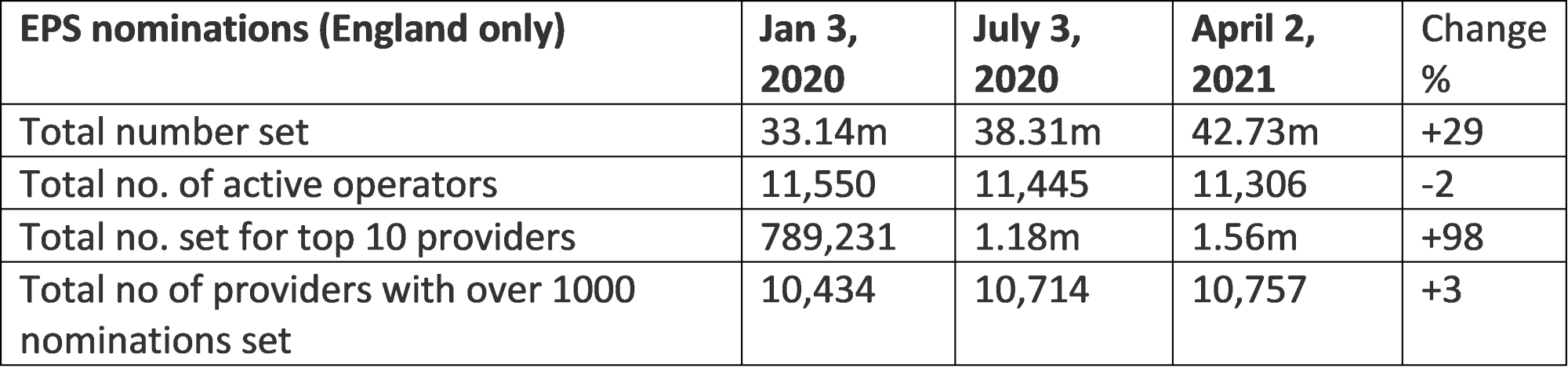
Before COVID, demand for digital prescription services was growing but relatively insignificant. However, lockdown has changed all that: in the period from pre-lockdown to latest figures available at the time of writing (Jan 3, 2020- April 2, 2021) there has been a 30 per cent increase in use of the electronic prescription service in England, a process that allows people to digitally nominate pharmacies, including mail order businesses, to fulfil their prescriptions. Latest figures show that of the top 10 pharmacies nominated to handle EPS scripts, two online only operators alone accounted for just over one million EPS nominations, and collectively grew their business by over 3,800 nominations in just one week.
Online pharmacy Mypharmacy.co.uk has reported that between 2018 to February 2020, the business observed steady year-on-year growth of around 10 per cent. However, during the lockdown period March 2020 - July 2020 online sales increased by 50 per cent, with a 45 per cent increase in customer numbers.
More evidence for the move online is available from The Health Foundation that shows that during the first lockdown, some 45 per cent of UK adults ordered a repeat prescription online and 21 per cent used email/text/app for communicating with a healthcare professional.
A recent paper from consultant Deloitte concludes: “The pandemic is rapidly changing our behaviour toward online channels, and the shifts are likely to stick post-pandemic", citing convenience and greater choice as just two of the reasons consumers will continue to shop online.
Rural roadmap
It’s a moot point whether lockdown healthcare practices will continue throughout, and after, the lockdown recovery period in rural areas where the demographic is older and where digital illiteracy and/or lack of connectivity is more prevalent than in urban areas.
In a recent rural proofing toolkit, Rural England suggests that traditional dispensing GP services such as prescriptions delivered to village shops for remote collection may present a solution to the unique challenges of delivering healthcare services in remote and rural areas, where technology, for whatever, reason cannot fill the gap.
Mohammed Yasir, who runs a traditional bricks and mortar pharmacy in Lancashire alongside the mypharmacy.co.uk online business, agrees that face-to-face pharmacy services have a role moving forward, albeit in a more customer-centric, service-focused way.
Many of the unique services offered by dispensing GP practices – home/remote prescription delivery services, patient’s dispensed medication reviews – are often subsidised by the income provided by the GP dispensing service. For this reason, PNA planners may wish to take note of the unique role these services play in rural communities, when considering the adequacy of their local pharmaceutical network.
NATIONAL CENTRE UPDATE
Parliamentary Inquiry
The first full draft of the write up of the Parliamentary Inquiry is now completed in draft form. We anticipate being able to share the headline findings with the Parliamentary Inquiry stakeholders in June.
Rural Proofing Toolkit Update
We have interest from Lincolnshire and Devon ICS in trialling this toolkit but would really welcome additional expressions of interest in joining in the process of testing.
Defra Discussions:
As a consequence of discussions at the Rural Coalition (of which the National Centre is a member) the centre has entered a dialogue with Defra to identify how we might support their feed into DHSC as part of their rural proofing responsibilities. We have identified that there are 4 core areas of relevance where the National Centre has made progress:
- Finance
- Workforce
- The IMD Research
- The Differential Impact on Health Systems in Rural Area
We are currently developing a briefing note to support the dialogue with Defra.
Membership and Website Round Up
Membership numbers are holding up well for the centre. We are planning a refinement of the website which will be more accessible and dynamic. Watch this space!!!
NHS Confederation MoU Progress
Following the agreement of a joint working MoU with the NHS Confed a community of practice and June launch event are being planned. We will be in touch with more information very soon.
FUNDING OPPORTUNITIES
This month we focus on Innovate UK but be quick the closing date 26 May 2021! To find out more about each of these funds click here
Spread the word
If you know of other organisations that you think would benefit from joining the Rural Health & Care Alliance, please click here to email us and let us know.
RURAL SERVICES NETWORK
Up to date news on Health and Care
The Rural Services Network provides a useful source of themed news content and data. Check out the latest news on Health & Wellbeing and Vulnerability, where you’ll find articles on a diverse range of rural issues affecting rural communities. You might also find this research on Over 65 Population Projections useful too.
Latest from RSN Member Insights
RSN Member Insights is the place to discover the statistics that define communities within our membership. It is regularly updated with new analyses, and these will be highlighted in the 'What's New' section of the RSN's Weekly Rural Bulletin. The Rural Bulletin also provides a selection of the most rurally topical news items, so do subscribe and encourage your colleagues to subscribe to what is an invaluable weekly periodical.
To make a suggestion of data that would benefit you by being included in the Member Insights section, please email Dan Worth, our Research and Performance Analyst, at [email protected].
| The Rural Health & Care Alliance is a membership organisation administered by the Rural Services Network on behalf of the National Centre for Rural Health & Care. Explore the RHCA service below: |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |





