T: 01822 851370 E: [email protected]
Visit RSN Survey about life in rural England to find out more.
November Edition of Casebook from the Rural Health and Care Alliance
November 2021 Edition
In Casebook this month it seems like the pandemic, which is raging through bits of Europe at the moment has some long-term negative legacy issues for rural communities. These underpin many of the stories in this edition of Casebook.
NEWS COMMENTARY
Covid: WHO says it is very worried about Europe surge
This article reminds us of the resilience of the virus. I am still very nervous about what a further wave might mean for people in isolated rural communities. This story tells us:
The World Health Organization (WHO) is "very worried" about the spread of Covid-19 within Europe as the continent battles a fresh wave of infections.
Speaking to the BBC, regional director Dr Hans Kluge warned that some 500,000 more deaths could be recorded by March unless urgent action is taken.
Dr Kluge said introducing measures like mask wearing could immediately help.
The warning comes as several nations report record-high infection rates and introduce full and partial lockdowns.
Dr Kluge said factors like the winter season, insufficient vaccine coverage and the regional dominance of the more transmissible Delta variant were behind the spread. He called for increased vaccine uptake and the implementation of basic public health measures and new medical treatments to help fight the rise.
"Covid-19 has become once again the number one cause of mortality in our region," he told the BBC, adding "we know what needs to be done" in order to fight the disease.
Dr Kluge said mandatory vaccination measures should be seen as a "last resort" but that it would be "very timely" to have a "legal and societal debate" about the issue.
Full article: https://www.bbc.co.uk/news/world-europe-59358074
Deaths of people treated under the Mental Health Act rose during pandemic
This is a worrying story. People from rural areas in these settings are more isolated and removed from their families and support groups and this situation has clearly ben exacerbated by the pandemic.
The number of deaths of people being treated under the Mental Health Act in England rose during the coronavirus pandemic, estimates suggest.
The Care Quality Commission's (CQC) findings come amid concerns over staff shortages in psychiatric units.
Some 490 people died while detained under the act in the year to March 2021 - 324 of them for non-Covid reasons, the regulator says.
BBC analysis found the average overall figure between 2012 and 2019 was 273.
Former Conservative Health Secretary Jeremy Hunt warned that staff shortages were now compromising patient safety in "every part of the NHS".
He called the figures on deaths in psychiatric detention "very concerning", but added: "It's not just mental health, but every specialty now has shortages of doctors and nurses."
Mr Hunt argued a "radical overhaul" of the training system was needed to ensure there were enough doctors and nurses in the coming decades.
Full article: https://www.bbc.co.uk/news/uk-politics-59336579
Six in 10 elderly care users in England set to lose out from change to costs cap
With a skewed demography in rural England, meaning a higher proportion of people in elderly care settings this reads like potential bad news for those of the most modest means. The story tells us:
The key architect of the government’s social care reform has said most older people needing care will lose out from plans to dilute protections against crippling costs in England, as Conservatives blamed Rishi Sunak for forcing the changes.
Sir Andrew Dilnot, an economist who devised reforms to prevent people losing homes to soaring care costs, told MPs on Thursday that he was very disappointed by a change to the way the cap on care costs was expected to work that would leave anyone with assets of less than £186,000 – about 60% of older people needing care – less well-off than expected.
On Wednesday the care minister, Gillian Keegan, announced that state-funded care costs would not go towards the new £86,000 cap – announced by Boris Johnson in September – on the amount anyone in England would pay for social care.
It will save the government hundreds of millions of pounds but leave many poorer homeowners exposed to “catastrophic costs” including the need to sell their homes to cover long-term care, analysts have said.
Whitehall sources confirmed that budget constraints imposed by the Treasury were behind the shift, saying, “cost is absolutely a factor”.
One senior former minister said the move was “absolutely Treasury driven”, and said Sunak was fixated on “trying to do the finances first and then work out what you need to do to actually solve the problem which – in this case – they haven’t addressed yet at all.”
Full article: https://www.theguardian.com/society/2021/nov/18/six-in-10-elderly-care-users-in-england-set-to-lose-out-from-costs-cap
A&E waits ‘kill’ as long delays drive thousands of patient deaths
This aspect of the backwash from covid is clearly having a major impact and I suspect has led to a fair proportion of these deaths being linked to people in rural settings. This story tells us:
Long delays and overcrowding in A&Es “kill” and may have caused thousands of patient deaths during the pandemic, a new report has revealed.
The Royal College of Emergency Medicine has sent a stark warning that patients will come to “avoidable harm” in A&Es across the country after it estimated, 4,519 patients are likely to have died after waiting more than 12 hours in emergency departments during 2020-21.
The news comes following record levels of 12 hour A&E waits, sometimes called trolley waits, with more than 7,000 patients waiting in October. However, the real numbers of people waiting is likely to be more than 20 times higher.
According to the Royal College of Emergency Medicine (RCEM), 300,000 patients waited more than 12 hours from the time they arrived in A&E in 2020-21, while monthly NHS data for the year only recorded around 14,000. This is because monthly figures only look at the length of time patients wait after staff have decided to admit them.
The report warned: “It is a vicious and dangerous cycle whereby crowding causes longer waits to treatment for patients, and consequently these longer waits further contribute to crowding in EDs. This is also a serious safety concern for patients who may initially appear well but have a serious underlying cause for their presentation.”
Full article: https://www.independent.co.uk/news/health/a-e-delays-kill-thousands-patient-deaths-b1959558.html
Rollout of third Covid jabs in England condemned as ‘shambolic’
Worrying stuff. This article does make me think more widely about the really important role the voluntary sector has played in supporting the roll out of the vaccine, not just speaking up for key groups but helping with the running of vaccination centres as well.
A “shambolic” rollout of third Covid vaccinations has left an unknown number of immunocompromised people still without proper protection going into winter, and in other cases even given the wrong type of injection, a leading charity has said.
Blood Cancer UK said poor planning and confusing messaging meant “many thousands” of people with weakened immune systems might have missed out, leaving them at greater risk of serious consequences if they catch Covid.
In a lengthy statement, the charity said NHS England had repeatedly failed to acknowledge the problem, while Sajid Javid, the health secretary, incorrectly said more than six weeks ago that the “vast, vast majority” of eligible people had already been invited for a third jab.
People were still coming forward to say they were struggling to get a third dose, said Gemma Peters, the chief executive of Blood Cancer UK. “The rollout of the third doses has been shambolic, causing yet more anxiety for immunocompromised people.”
Third doses are separate to the wider programme of booster jabs, now being extended to adults aged 40 and above. Third injections are aimed at increasing the protection for people whose immune systems have been affected by conditions including blood cancer, with Covid vaccines likely to be less effective for them.
Full article: https://www.theguardian.com/society/2021/nov/18/rollout-third-covid-jabs-england-condemned-shambolic
MEMBER ARTICLES
We’d love to hear from you - share what you’re proud of
If you have something you would like us to feature in a future edition, please let us know by clicking here to send us an email.
This month we hear from two NHS Foundation Trust members, read on:
 |
Facility Improvements and Community Promise
Northumbria Healthcare NHS Foundation Trust is one of the largest NHS trusts in the country and provides services to more than 500,000 people across the 2,500 square mile area of Northumberland and North Tyneside. Staff provide care in an emergency care, general and community hospitals, via a range of community services and in people’s own homes.
 Last month, Guy Opperman MP unveiled a plaque at Hexham General Hospital to mark the opening of the MRI scanner facility.
Last month, Guy Opperman MP unveiled a plaque at Hexham General Hospital to mark the opening of the MRI scanner facility.
The state-of-the-art machine has actually been in operation for more than 18 months now, with the original plans for an opening ceremony put on hold due to the pandemic.
Since opening, the service, operating three days a week, is seeing around 300 patients every month for key diagnostic scans, including around 25 cardiac patients per month undergoing specialised scans and 15 arthrograms – high-tech imaging for musculoskeletal conditions.
The hospital serves a large rural hinterland in the west of Northumberland, meaning timely access to the latest world-class technology much closer to home for many, not just in Northumbria Healthcare’s catchment, but across a wider, fairly remote area with limited access to MRI facilities.
Watch a video about the MRI scanner and what it means for patients here:
 In the far north of the Northumbria patch, good progress continues to be made on the new, state-of-the-art £30million hospital at Berwick. The latest phase of the development, which will ensure modern and fit-for-purpose healthcare for a population spread another large rural area, this time in north Northumberland, is the demolition of parts of the existing infirmary, which dates back almost 150 years.
In the far north of the Northumbria patch, good progress continues to be made on the new, state-of-the-art £30million hospital at Berwick. The latest phase of the development, which will ensure modern and fit-for-purpose healthcare for a population spread another large rural area, this time in north Northumberland, is the demolition of parts of the existing infirmary, which dates back almost 150 years.
Buildings including theatres, the day ward, the reception, outbuildings and the energy centre will be demolished in a carefully managed sequence, taking into account the archaeological work that continues on site. A major dig is under way after discoveries during initial work carried out as part of the planning process. The team has uncovered what appears to be cobbled yards, a well and artefacts, including pottery, dating back to medieval times – around 1100AD, providing valuable insight into the history of the town.
Construction of the new hospital is planned to start in the spring of 2022.
Serving a diverse range of rural and urban populations means that we are focused on the issue of health inequalities and how they affect our communities. To this end, we have created a Health Inequalities Programme Board, chaired by leading public-health consultant Jonny Pearson-Stuttard, to lead our efforts on this, building on key regional partnerships.
 In addition, earlier this year, we launched Our Community Promise, our pledge to make a difference to the people who live here, not just through providing high-quality healthcare, but by dealing with many of the social determinants of health and the ways we can have an impact, such as education, employment and the economy, factors which affect both rural and urban populations in different but equally serious ways.
In addition, earlier this year, we launched Our Community Promise, our pledge to make a difference to the people who live here, not just through providing high-quality healthcare, but by dealing with many of the social determinants of health and the ways we can have an impact, such as education, employment and the economy, factors which affect both rural and urban populations in different but equally serious ways.
Our Community Promise is introduced here
 |
Addressing rural health inequalities as an anchor institution
Dorset County Hospital is the main provider of acute hospital services, and the largest employer, in West Dorset. As well as providing health services to our local community, we employ over two and a half thousand people; we spend millions of pounds each year on goods and services and have a major impact on our local environment. As such, we are an anchor institution and have an important role to play in both the social and economic development of our communities following the pandemic. Fundamental to this is our hospital’s Social Value pledge which commits to reduce avoidable inequalities and improve health and wellbeing across our community.
As an Acute hospital, serving a largely rural population, we face key challenges including an ageing population, 29% of Dorset’s population are 65 years and over, predicted to grow by 34% in the next 5-8 years. We serve hard to reach, isolated communities with weak transport links and lengthier travel times to reach hospital; compounded by digital exclusion. Recruitment and retention of healthcare professionals is difficult due to a lack of working age people and outward migration of younger people. We face increased financial pressures, having to deliver the same level of quality whilst undertaking small activity numbers; and productivity challenges working across multiple sites including community hospitals. Our local coastal communities have some of the highest levels of social deprivation nationally. Read more
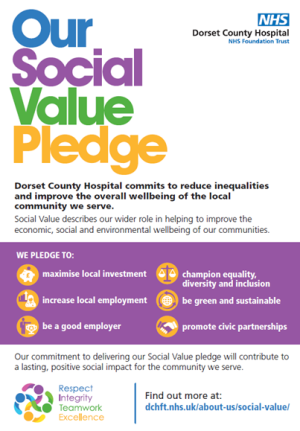 As an NHS anchor institution we have a responsibility, and the capacity, to help proactively address health inequalities across our region. Health inequalities were prevalent prior to the pandemic, particularly across rural communities. COVID-19 has highlighted and exacerbated these inequalities. The pandemic has had a disproportionate, detrimental impact on people living in rural areas of high deprivation, ethnic minority communities, those with learning disabilities and others with protected characteristics and older people. To overcome this inequity and build back fairer will require a new approach to levelling up to tackle inequalities. We need a different relationship with the community, providing a wrap-around service which delivers outstanding healthcare, whilst also improving the socio-economic well-being of the population we serve. For Dorset County Hospital our social value programme is the cornerstone of this ambition. We have committed to deliver on our pledge to procure more goods locally, supporting local businesses; increase local employment through targeted recruitment and schemes such as the Kickstart programme; by supporting the well-being of our workforce as a good employer; to champion equality, diversity and inclusion and by improving our environmental sustainability contributing to the NHS Net-zero goals. We are also working with our Dorset ICS partners and other civic partners to develop a system-level approach to improving health equity and the wider social, economic and environmental vitality of our region.
As an NHS anchor institution we have a responsibility, and the capacity, to help proactively address health inequalities across our region. Health inequalities were prevalent prior to the pandemic, particularly across rural communities. COVID-19 has highlighted and exacerbated these inequalities. The pandemic has had a disproportionate, detrimental impact on people living in rural areas of high deprivation, ethnic minority communities, those with learning disabilities and others with protected characteristics and older people. To overcome this inequity and build back fairer will require a new approach to levelling up to tackle inequalities. We need a different relationship with the community, providing a wrap-around service which delivers outstanding healthcare, whilst also improving the socio-economic well-being of the population we serve. For Dorset County Hospital our social value programme is the cornerstone of this ambition. We have committed to deliver on our pledge to procure more goods locally, supporting local businesses; increase local employment through targeted recruitment and schemes such as the Kickstart programme; by supporting the well-being of our workforce as a good employer; to champion equality, diversity and inclusion and by improving our environmental sustainability contributing to the NHS Net-zero goals. We are also working with our Dorset ICS partners and other civic partners to develop a system-level approach to improving health equity and the wider social, economic and environmental vitality of our region.
As we progress we will evaluate and report on our social value outcomes and our impact on reducing avoidable inequalities as an anchor institution. As we move beyond the pandemic, we aim to create a lasting, positive social impact, improving the overall well-being of the communities we serve.
NATIONAL CENTRE UPDATE
Parliamentary Inquiry
We are just checking the draft report with witnesses but anticipate that we will launch the full document in January, taking account of the Christmas break in Parliament. We are thrilled with progress. A number of key partners including the Rural Services Network and Rural Coalition have agreed to put their weight behind driving its recommendations home as strongly as possible.
Rural Proofing Toolkit
There is growing interest in this facility in partners in Northern Ireland. We held a briefing session on Friday 19th November which was well attended and garnered really strong enthusiasm for engaging with the process of rolling the toolkit out in their area and joining the learning set we are working on. Just goes to show we strong the universal principles we have built into the toolkit are bearing in mind it was designed for an English context.
Social Valu
We have found an increasingly strong interest amongst members in relation to social value. Over the next few months, we hope to be able to produce a deal providing interested parties within our membership with low-cost access to an accredited on line tool.
FUNDING OPPORTUNITIES
This month we focus on four funding streams including:
1. Warm Homes Fund Reopens – to improve health and tackle fuel poverty
2. Emergency Grants Programme – to support Afghan Evacuees
3. Family Hubs Transformation Fund – seeking applications from local authorities
4. Music Grants for Older People – relevant to charities and care homes.
To find out more about each of these funds click here
Spread the word
If you know of other organisations that you think would benefit from joining the Rural Health & Care Alliance, please click here to email us and let us know.
RURAL SERVICES NETWORK
Up to date news on Health and Care
The Rural Services Network provides a useful source of themed news content and data. Check out the latest news on Health & Wellbeing and Vulnerability, where you’ll find articles on a diverse range of rural issues affecting rural communities. You might also find this research on Over 65 Population Projections useful too.
Latest from RSN Member Insights
RSN Member Insights is the place to discover the statistics that define communities within our membership. It is regularly updated with new analyses, and these will be highlighted in the 'What's New' section of the RSN's Weekly Rural Bulletin. The Rural Bulletin also provides a selection of the most rurally topical news items, so do subscribe and encourage your colleagues to subscribe to what is an invaluable weekly periodical.
To make a suggestion of data that would benefit you by being included in the Member Insights section, please email Dan Worth, our Research and Performance Analyst, at [email protected].
| The Rural Health & Care Alliance is a membership organisation administered by the Rural Services Network on behalf of the National Centre for Rural Health & Care. Explore the RHCA service below: |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |




