T: 01822 851370 E: [email protected]
Visit RSN Survey about life in rural England to find out more.
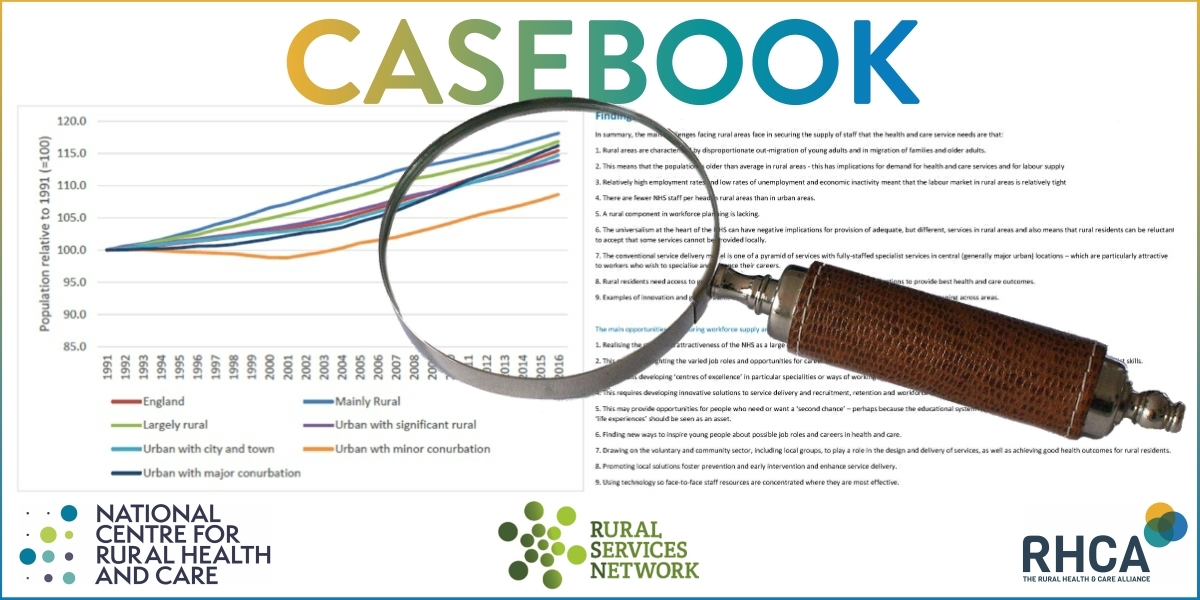
September Edition of Casebook from the Rural Health and Care Alliance
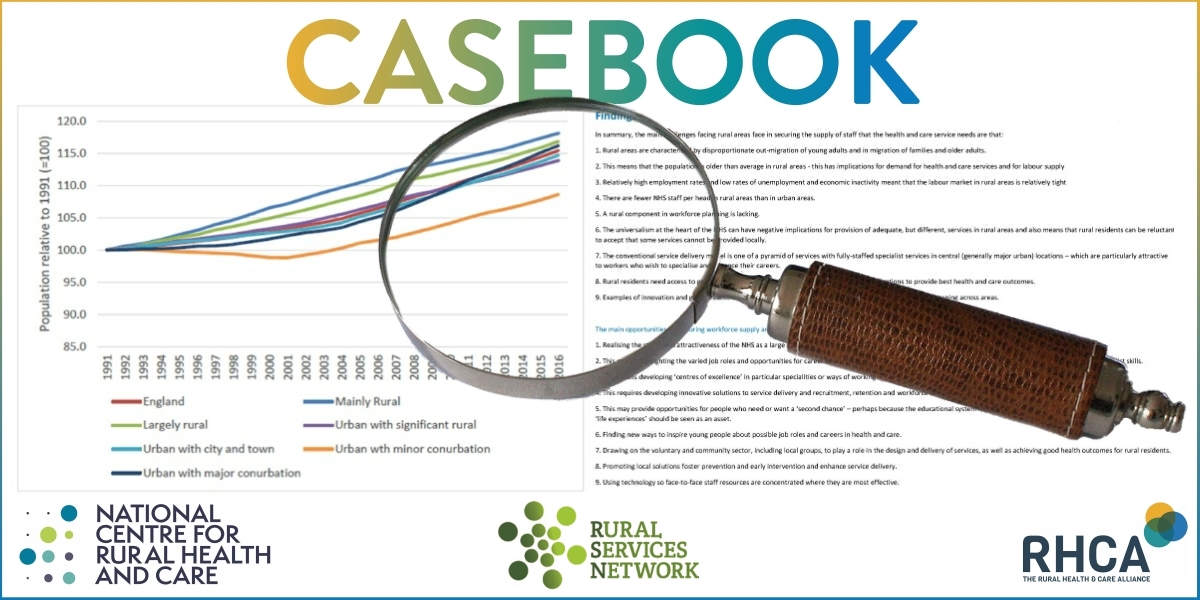 September 2025 Edition
September 2025 Edition
Welcome to this month’s edition of Casebook. We explore the ongoing challenges of rural service delivery, the introduction of national NHS league tables, and the continuing shortfall in health provision for rural areas. On a more positive note, we share best practice from the National Rural Conference, along with practical tips on tackling inequalities and building resilience. Finally, we’re delighted to invite you to our next Rural Health and Care Seminar this November, featuring another fantastic line-up. Read on!
Rural Health and Care: Unequal Access and Community Solutions
 This year’s RSN National Rural Conference dedicated a session to the pressing issue of rural health and care, with speakers exposing persistent inequalities while showcasing community-driven solutions that are beginning to make a difference.
This year’s RSN National Rural Conference dedicated a session to the pressing issue of rural health and care, with speakers exposing persistent inequalities while showcasing community-driven solutions that are beginning to make a difference.
Opening the session, RSN Chief Executive Kerry Booth reminded delegates of the government’s stated ambition to bring more care into communities, harness digital tools and place greater emphasis on prevention. Yet, she stressed, these shifts are far from reality in the countryside: only 81% of rural residents can reach a GP within 30 minutes, ambulance response times are on average 67% longer than in towns and cities, and rural adults are significantly less likely to have accessed an NHS dentist in the last two years
Against this backdrop, Dr Christina Dobson of Newcastle University presented sobering findings on cancer outcomes. Rural patients remain 5% less likely to survive cancer than urban patients, a gap that has persisted for more than three decades. Her research highlights the many reasons why—from long travel times for screening and treatment, to seasonal work that delays appointments, to the erosion of long-standing GP–patient relationships that once gave reassurance and continuity
The discussion then turned to the hidden issue of domestic abuse. Judith Vickress, Churchill Fellow, painted a stark picture of how isolation and stigma in rural areas can be weaponised by abusers, leaving victims with little space to seek help. She called for a coordinated community response, where neighbours, local groups, health services and the police work together so no one is left behind because of where they live
Looking to the future, Dr Tim Sanders from The University of Lancashire and Dr Chris Ford from Lancaster University presented the Penrith case study, showing how rural hub towns can act as “keystones” for surrounding areas. By reimagining town centres as ecosystems linking health, culture, economy and the environment, they argued, hub towns can become anchors for wellbeing, regeneration and connection
Finally, Lisa Farley of Young Somerset offered an uplifting example of change already happening. The “Right Time, Right Support” model for young people’s mental health has slashed waiting times, with 86% now seen within four weeks compared to just 13.7% before reforms. In the past year alone, her team delivered more than 8,000 interventions, with overwhelmingly positive feedback from young people and families
The session closed with a panel discussion chaired by Kerry Booth where delegates reflected on the challenges laid bare, unequal access, stretched services, and hidden harms but also on the creativity and determination of rural communities in building solutions.
Rural Health Gaps Widening
 The newly published State of Rural Services 2025 report from Rural England CIC shows that health inequalities remain a defining challenge for rural communities. Despite some improvements in digital delivery, access to face-to-face care continues to lag behind urban areas.
The newly published State of Rural Services 2025 report from Rural England CIC shows that health inequalities remain a defining challenge for rural communities. Despite some improvements in digital delivery, access to face-to-face care continues to lag behind urban areas.
Primary care pressures are evident. The number of GP surgeries in rural England fell by 15.5% between 2013 and 2024, with closures increasing travel distances. For people living in villages, hamlets and isolated dwellings, the average minimum journey to a GP is at least 57 minutes by public transport or walking. Continuity of care is also declining, with very few permanent GPs remaining in the same post long-term in predominantly rural areas.
Dentistry and pharmacy services are similarly stretched. Only 38% of adults in rural areas saw an NHS dentist in 2022/23, compared with 45% in urban areas. There are just 50 NHS dentists per 100,000 people in rural areas, and provision is heavily concentrated in larger settlements. Pharmacies have also seen closures and reduced hours, leaving many smaller communities reliant on travel.
Hospital and emergency provision is under pressure. The number of rural hospitals has fallen by 35% in the past 15 years, with only 75 now remaining in England. Most are located in less remote “town and fringe” areas. Ambulance response times are significantly slower in rural places, further compounding the risks posed by distance.
The report also highlights older people’s care as a pressing issue. Just 1,706 registered care homes are located in rural England, with the majority clustered in larger or less remote communities. This leaves many older residents facing the prospect of moving away from long-standing homes and social networks to access appropriate care.
While data on mental health remains limited, existing evidence points to increased risks of isolation, depression and stress in farming households and remote settlements, with poor transport and patchy internet access restricting engagement with support services.
The conclusion is clear: many rural communities still lack even the basics of healthcare infrastructure, from GP surgeries and pharmacies to care homes and hospitals. The report calls for policymakers to take these disparities seriously to ensure rural residents are not left behind.
Read the full State of Rural Services 2025 report here
Macmillan Highlights Major Gaps In UK Cancer Treatment
 Macmillan Cancer Support has warned that almost 1.4 million people with cancer in the UK are being failed by what it describes as a “cancer postcode lottery”.
Macmillan Cancer Support has warned that almost 1.4 million people with cancer in the UK are being failed by what it describes as a “cancer postcode lottery”.
New research from the charity, one of the UK’s leading providers of cancer information, advice and support, shows that 40% of people with cancer have struggled to access tests, treatment, or care because of where they live. This inconsistency in services means some patients face long journeys, additional costs, stress and fatigue, while others risk missing out on potentially life-saving treatment altogether.
Macmillan’s analysis suggests that if all areas of the UK matched the performance of the best-performing regions, around 60,000 more people each year would start cancer treatment on time. At its most extreme, the postcode lottery could put an estimated 100,000 lives at risk, as some patients have turned down tests or treatment due to travel distances.
The charity highlights that variation is not only affecting access to established treatments but also the roll-out of innovative new options, with implications for outcomes, recovery and long-term quality of life.
Macmillan is calling for urgent action from governments and health systems across the UK to address these inequalities and ensure everyone with cancer receives the best possible care, regardless of where they live.
Read more here |
The full analysis is available here |
Landmark NHS League Tables Rolled Out
 A new system of NHS league tables has been launched across England, with every trust now ranked quarterly against clear standards covering urgent and emergency care, planned operations, mental health and ambulance services.
A new system of NHS league tables has been launched across England, with every trust now ranked quarterly against clear standards covering urgent and emergency care, planned operations, mental health and ambulance services.
The government says the reform marks a “new era of transparency and accountability” in the NHS. Trusts will be grouped into four performance segments: the best-performing will gain greater autonomy and the ability to reinvest surplus budgets in local improvements such as diagnostic equipment or hospital upgrades, while the most challenged will receive targeted support. Senior managers will also be held accountable through performance-linked pay, and patient feedback will form part of the assessment.
Separate tables are being published for acute, non-acute and ambulance trusts. By 2026, the system will expand to include integrated care boards, which are responsible for planning health services for local populations. NHS England has stressed that the differences between organisations placed close together in the rankings may often be marginal, and that the tables should be used as a guide rather than a definitive judgement.
For rural communities, the approach could highlight how geography and access pressures affect performance, and where extra support is most needed to ensure services meet the needs of patients in dispersed areas.
The reform is part of the government’s 10 Year Health Plan and follows wider measures under the Plan for Change, including action to reduce waiting lists and expand GP numbers.
Read the full announcement here
Persistent ‘Dental Deserts’ Risk Leaving Rural Communities Behind
 New analysis from the Local Government Association (LGA) highlights a continuing crisis in NHS dental provision, with so-called ‘dental deserts’ leaving many communities – particularly rural and deprived areas – struggling to access care.
New analysis from the Local Government Association (LGA) highlights a continuing crisis in NHS dental provision, with so-called ‘dental deserts’ leaving many communities – particularly rural and deprived areas – struggling to access care.
Using NHS England data, the LGA found that no local authority area in England has more than one NHS dentist per 1,000 residents. Rural areas in particular are more likely to have fewer practices, creating significant barriers to treatment.
The analysis also reveals striking inequalities:
- Communities with the poorest health outcomes are less likely to find an NHS dentist locally than those with the best outcomes.
- Middlesbrough, one of the most deprived areas in England, has just 10 NHS dental practices per 100,000 people, compared to 28 per 100,000 in affluent Richmond upon Thames.
- Areas with high levels of child dental decay do not necessarily have better NHS provision than areas with lower levels.
The LGA warns that this unequal distribution is widening health inequalities, and is calling on Government to introduce targeted measures to improve access where need is greatest.
Cllr Dr Wendy Taylor, Chair of the LGA Health and Wellbeing Committee, said:
"There is still a shortage of affordable dental treatment in all communities across the country, particularly rural and more deprived areas. Poor dental health can significantly impact overall health outcomes, including cardiovascular disease. Equal access to NHS dental services is vital for every community".
British Dental Association Chair, Eddie Crouch, added:
"For millions, NHS dentistry has effectively ceased to exist, especially among those who need care the most. Government can save this service, but that will require real ambition underpinned by sustainable funding".
The LGA welcomed recent steps by Government to expand provision and invest in community dental services but argues that a fundamental review of the NHS dental contract is essential to secure long-term, equitable care.
Thousands More Checks, Tests And Scans Now Available Out Of Hours
 The Department of Health and Social Care has announced that 100 Community Diagnostic Centres (CDCs) across England are now offering out-of-hours services, open 12 hours a day, seven days a week.
The Department of Health and Social Care has announced that 100 Community Diagnostic Centres (CDCs) across England are now offering out-of-hours services, open 12 hours a day, seven days a week.
The government says this milestone will allow tens of thousands more patients to access vital tests, scans and checks around busy working lives. Since July 2024, over 1.6 million additional tests and scans were delivered compared to the previous year — and now 100 out of 170 CDCs in England offer extended opening hours (NHS England statistics).
Community Diagnostic Centres are designed to bring services closer to people’s homes by being sited in accessible locations such as shopping centres, university campuses, football stadiums or community hospitals (NHS England – CDC overview).
While the expansion of opening hours offers greater flexibility, the accessibility of these centres for people living in rural areas remains a key question.
Analysis from the Independent Healthcare Providers Network shows that only a limited number of CDCs are located in fully community-based venues such as retail parks or standalone hubs, while many more continue to operate from hospital or community hospital sites (IHPN report, 2024). For rural residents, this may still mean substantial travel, especially given that diagnostic facilities are historically less available in rural areas.
CDC services also depend on digital systems for referrals, appointment booking and results. For rural residents, connectivity remains a barrier:
- Despite investment, thousands of households in rural England still lack access to fast and reliable broadband, which is essential to support digital health systems.
- The King’s Fund has previously noted that CDC effectiveness is linked to strong IT infrastructure, raising questions about whether areas with weaker digital foundations can fully benefit.
- Telehealth usage in rural areas remains lower than in urban counterparts, with digital connectivity and digital literacy both identified as key factors (BPP Care, 2024).
The expansion of CDC opening hours is a positive step in the NHS’s plan to improve access and reduce backlogs. However, for rural residents the full benefits will depend on how far centres are genuinely accessible without long travel, and whether digital infrastructure keeps pace to support smooth referrals and results.
Upcoming events
Book onto the upcoming Rural Health and Care Seminar by clicking below:
We’d love to hear from you - share what you’re proud of
If you have something, you would like us to feature in a future edition, please let us know by clicking here to send us an email.
Spread the word
If you know of other organisations that you think would benefit from joining the Rural Health & Care Alliance, please click here to email us and let us know.
RURAL SERVICES NETWORK
Up to date news on Health and Care
The Rural Services Network provides a useful source of themed news content and data. Check out the latest news on Rural Access to Health and Care Services and Vulnerability, where you’ll find articles on a diverse range of rural issues affecting rural communities.
Latest from RSN Member Insights
RSN Member Insights is the place to discover the statistics that define communities within our membership. It is regularly updated with new analyses, and these will be highlighted in the 'What's New' section of the RSN's Weekly Rural Bulletin. The Rural Bulletin also provides a selection of the most rurally topical news items, so do subscribe and encourage your colleagues to subscribe to what is an invaluable weekly periodical.
| The Rural Health & Care Alliance is a membership organisation administered by the Rural Services Network on behalf of the National Centre for Rural Health & Care. Explore the RHCA service below: |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |




