T: 01822 851370 E: [email protected]
Visit RSN Survey about life in rural England to find out more.
February Edition of Casebook from the Rural Health and Care Alliance
February 2022 Edition
In Casebook this month, changing covid rules, hospital beds, racial inequalities, backlogs, workforce and the publication of our own Parliamentary Inquiry. Read on…
NEWS COMMENTARY
Is ending the last Covid rule 'brave or stupid'?
I really don’t know which way to swing on this, what do you think? Should we be relaxing, or shouldn’t we? The article tells us:
With new treatments and a huge amount of immunity in the population, from both vaccination and infection, the risk from the virus is lessening all the time.
Other nations are also relaxing rules around self-isolation. Denmark, for example, now requires people to stay at home only if they have symptoms.
Nonetheless, there are also grounds for caution. Infection levels remain high.
And the Office for National Statistics (ONS) monitoring programme suggests they may even be rising again, with about one out of every 19 people in England positive last week.
Coupled with this is the rise of a sub-variant of Omicron, BA.2, thought to be even more transmissible than the version, first identified in South Africa, that caused the Christmas surge. BA.2 now accounts for an estimated one out of every six infections - a proportion that is growing every week.
This is one of the reasons Prof Paul Hunter, an expert in infectious disease, at the University of East Anglia, was surprised by the announcement on self-isolation.
"At some point, it is going to be the case that all remaining restrictions are dropped, including the need to self-isolate, though I certainly didn't expect that to happen this month," he says.
Prof Hunter would have preferred to wait a little bit longer to see what happens with infections and the sub-variant.
Full article: https://www.bbc.co.uk/news/health-60324928
Sickest face record long waits for hospital bed
This is a disproportionately huge issue for rural dwellers who have the furthest to travel and the fewest ongoing travel options connected to the A&E experience.
The sickest patients are facing long waits for a bed when they are admitted to hospital in England, NHS data shows.
A third of the A&E patients - 122,000 in total - who were ill enough to need treatment on a ward waited over four hours in January - a record high.
Some 16,500 of them waited over 12 hours - many either stuck on trolleys in corridors or in A&E bays because wards were full.
Doctors warned the situation was putting patients at risk.
These patients are ones who will have already faced a wait to be seen in A&E, but need further treatment because their condition is so serious.
The NHS England figures also showed cancer waiting times have hit their worst level since records began, with only two-thirds of patients starting treatment within the target time of two months following an urgent GP referral.
Meanwhile, the numbers of people on hospital waiting lists for planned treatments has risen to 6.1 million.
Earlier this week ministers set out a recovery plan to tackle the backlog in treatments, which includes people waiting for hip and knee replacements.
They warned the waiting list could keep rising for two years before starting to fall.
Waiting times have worsened in other parts of the UK, with Wales and Northern Ireland data showing even worse performance than England on many measures.
Full article: https://www.bbc.co.uk/news/health-60334081
Radical action needed to tackle racial health inequality in NHS, says damning report
This is a really important report – with implications that we should all take super seriously.
Radical action is needed urgently to tackle “overwhelming” minority ethnic health inequalities in the NHS, leading experts have said, after a damning study found the “vast” and “widespread” inequity in every aspect of healthcare it reviewed was harming the health of millions of patients.
Racism, racial discrimination, barriers to accessing healthcare and woeful ethnicity data collection have “negatively impacted” the health of black, Asian and minority ethnic people in England for years, according to the review, commissioned by the NHS Race and Health Observatory, which reveals the true scale of health inequalities faced by ethnic minorities for the first time.
“Ethnic inequalities in health outcomes are evident at every stage throughout the life course, from birth to death,” says the review, the largest of its kind. Yet despite “clear”, “convincing” and “persistent” evidence that ethnic minorities are being failed, and repeated pledges of action, no “significant change” has yet been made in the NHS, it adds.
The 166-page report, seen by the Guardian, is due to be published in full this week.
From mental health to maternity care, the sweeping review led by the University of Manchester paints a devastating picture of a healthcare system still failing minority ethnic patients despite concerns previously raised about the harm being caused.
Full article: https://www.theguardian.com/society/2022/feb/13/radical-action-needed-to-tackle-racial-health-inequality-in-nhs-says-damning-report
NHS backlog poses existential risk to Boris Johnson’s government
The big, but nevertheless important story that failed to knock “party-gate” off its perch.
It wasn’t the sort of coverage Sajid Javid was hoping for. “Is that all we get for £12bn?” thundered the front page of Wednesday’s Daily Mail. The source of its frustration was the health secretary’s admission in the Commons 24 hours earlier that the length of the waiting list for hospital care in England, which now stands at a record 6.1 million people, would continue its relentless rise until March 2024. Javid’s candour came while he was launching NHS England’s “elective recovery plan”, its strategy – endorsed by the government – for addressing and, it is hoped, ultimately reducing that colossal backlog of care. The £12bn a year the forthcoming 1.25% rise in National Insurance will raise via the new health and social care levy will help fund the work involved.
The plan itself is a classically NHS document: 49 pages featuring a blizzard of statistics, examples of hospitals using innovative ways of reducing patients’ waiting times for care and a raft of detailed proposals aimed at “increasing health service capacity ... prioritising diagnosis and treatment ... [and] transforming the way we provide elective care”. However, the bits of most relevance – politically for ministers and practically for patients – are the targets setting out when indecently, sometimes dangerously long, and historically unprecedented, delays for treatment – for new hips and knees, cancer care, heart operations and much else besides – will finally end. Under the NHS constitution patients have a “right” – now often merely theoretical – to receive such care within 18 weeks.
The key targets – which are really just aspirations – include ensuring that by July no one has been waiting more than two years, 18-month waits are eradicated by March next year and one-year waits – 306,996 patients have recently faced a delay of that magnitude – banished by March 2025, and that the waiting list starts shrinking by March 2024, two months before the next election.
Full article: https://www.theguardian.com/society/2022/feb/13/nhs-backlog-poses-existential-risk-boris-johnson-government
More medical school places is no cure-all for the UK’s shortage of doctors
This is a really thoughtful letter about the challenge of increasing workforce skills from a rural practitioner. It tells us:
Prof Rachel Jenkins’ letter (9 February) advocates for the expansion of medical school places in the UK, and this should indeed be a priority to preserve the medical workforce of the future. But since 2010, medical student numbers have increased by 31% – with only a 0.4% increase in positions for the clinical academics who train them.
Besides university staff and infrastructure, medical students require the support of junior doctors in their workplace-based placements. But this is impossible to provide, with increasing numbers of students on the wards coupled with the pressure on service provision. As a doctor in her first year of practice, I am dismayed to have to turn students away, but I am aware that they often do not have the support on the ward to achieve their curriculum outcomes.
We do medical students, junior doctors, medical academics and ultimately patients a disservice when we use medical student places, and the funding for them, as the only measure of the quantity of high-quality medical education that is able to be delivered in the UK.
Full article: https://www.theguardian.com/society/2022/feb/13/more-medical-school-places-is-no-cure-all-for-the-uks-shortage-of-doctors
MEMBER ARTICLES
We’d love to hear from you - share what you’re proud of
If you have something you would like us to feature in a future edition, please let us know by clicking here to send us an email.
This month we have 5 member articles and news of an exciting rural world health event in Ireland.
 |
Exploring barriers to accessing online health services in Devon
Independent community development charity Devon Communities Together is collaborating with community health and wellbeing organisation, Wellmoor, on NHSX’s Digital Inclusion Pioneers Programme, to explore and understand the barriers to accessing online healthcare services.
While the use of digital devices is increasing across all population groups, adoption of digitally enabled health care is not growing at the same rate. Funding has been received to support discovery work with people living in our most rural communities - with particular focus on those living in the most deprived areas and those most geographically distant from our acute hospitals.
The project team has already conducted an exploratory workshop and has since been using the intelligence gathered to plan the forthcoming research programme.
“The key focus will be older people in rural areas who are digitally excluded, unwilling to try online consultations, or who have tried online consultations with clinicians and who can share their experiences (positive and negative),” said Laura Dixon, Project Manager at Devon Communities Together, which works with communities across Devon on a wide range of projects and services, many of which directly support community health and wellbeing.
“Not everyone is aware that remote consultations are being offered more widely but for people living in rural areas, a video call could be a way of getting the health care they need without having to travel what may be a long distance, particularly if reliant on public transport.
“Of course, online consultations may not be for everybody, and it may be difficult for people who don’t have a computer, who don’t feel confident either using one for a video call or talking about their health issues this way. We are looking forward to exploring these challenges with a wide range of service users and stakeholders to get a deep understanding of the barriers and how they may be overcome.”
The specific pathways being focused on are: Chronic Respiratory Disease; COPD; Early Cancer diagnosis (screening and early referral); Gastroenterology; Maternity; Mental Health MSK (painful bone and joint conditions).
The outcomes from the project will inform the development of a Digital Inclusion Strategy for Devon whilst also giving healthcare providers confidence in taking immediate action to addressing barriers to digital access.
If you would like to find out more about the project, please contact Laura Dixon on [email protected] Tel: 07943 861420

 |
Rural GPs under pressure because governments fail to rural proof
Dispensing doctors’ income is under pressure from Government policy in two UK nations, as a result of insufficient rural proofing.
Dispensing GP surgeries are mainly located in rural locations, where a community pharmacy is not economically viable. Dispensing practices therefore provide a vital NHS service for rural populations, which typically, are older than urban populations.
Funding for rural medical services is fundamentally propped up by dispensing income. A Cost of Service analysis of dispensing practice has demonstrated that up to half of a dispensing practice’s income is derived from dispensing. Of this dispensing income, more than half is made up of dispensing fees.
In Scotland the principle of cross-subsidy of general NHS GP services by dispensing income is recognised and now enshrined in legislation controlling pharmacy applications in areas where dispensing GPs operate.
A recent initiative by the Welsh Government seeks to reduce the volume of prescriptions dispensed in Wales – and thus the dispensing fees it pays - in a cost-saving measure for the NHS. However, the review of dispensing volumes in community pharmacies takes no account of the whole range of funding mechanisms for dispensing GPs – only some of which are shared with pharmacies. Nor does the planned review take account of the higher costs of service delivery that are common among rural service providers, including dispensing GPs.
Faced with similarly increasing drug costs the health administration in England has also proposed a review of community pharmacy drug reimbursement which, as in
Wales will impact on those areas of funding that are shared with dispensing GPs.
Due to the highly urban nature of most pharmacies, this review also lacks rural proofing. A consequence of this is that there may be changes that adversely affect the overall financial situation of dispensing GPs. Analysis of dispensing practice funding finds that nearly 40 per cent of overall dispensing income is made up of drug reimbursement payments.
Loss-making dispensaries will have a profound effect on the viability of rural general practices and the delivery of healthcare services in rural areas. Reimbursement mechanisms should as far as possible be designed to prevent dispensing doctors dispensing prescriptions at a financial loss, and as far as possible, provide certainty of reimbursement to dispensing doctors.
 |
Rural district nursing is not for the faint-hearted
Worcestershire is a rural county of valleys, rivers and patchwork fields, bordered by the Malvern Hills. Surrounded by outstanding natural beauty, it is easy to forget the challenges those living in rural communities might face when accessing healthcare.
Herefordshire and Worcestershire Health and Care NHS Trust provides a range of services, including care and support at home through a variety of community-based teams which support both physical and mental health needs of its population. It includes its integrated Neighbourhood Teams which brings together a range of professionals including district nurses, therapists, GPs, and social care staff providing care and treatment to more vulnerable patients in their own homes. The aim is to deliver proactive and responsive care to reduce unnecessary hospital admissions or repeat GP appointments.
Alongside having to adapt to the challenges COVID has provided, staff in those Neighbourhood Teams working in the most rural parts of the county must also overcome the obstacles of working in a rural environment.
Beth Ferris, Senior Community Nurse, EBBI Neighbourhood Team said: “Rural district nursing is not for the faint hearted; every day can be a challenge. From the distance we travel, lone nursing, and to the skills required to meet a wide scope of patient care for the most vulnerable and isolated in society. We are professionals who use our experience, knowledge and autonomy in often complex circumstances.”
Working in counties prone to adverse weather conditions, including severe annual flooding, the Neighbourhood Teams must be able to adapt to changing routes, and make crucial decisions to provide vital healthcare, alongside ensuring their own safety.
Beth added: “We must have our wits about us for weather conditions; especially in the winter months when snow and/or floods could cause dangerous driving conditions. Patience, when we are held up in the summer months by tractors and trailers causing us to get behind in our workload.
“We feel tired yet reassured that no matter how challenging our day has been, we have made a positive difference to somebody's day, acknowledging tomorrow is another day which will be filled with learning opportunities.”
However, it is not only the poor weather conditions that can make the provision of rural healthcare more challenging
Beth said: “We must be proactive in rural areas by recognising the difficulty to find addresses like named rather than numbered properties. We must use our initiative to utilise apps on our phones or to stop and ask the local postman who is always a guaranteed help.
“It may be a day when we see no other members of our team but receive a reassuring call asking if we’re ok. The strength of the tremendous team back at base is often our first port of call when support or advice is needed.”
 |
Lincolnshire patient thanks new COVID service for saving his life
Patients who are a greater risk of becoming seriously unwell from COVID-19 have praised a new service designed to aid their recovery from the virus and keep them out of hospital.
United Lincolnshire Hospitals NHS Trust is one of the biggest acute hospital trusts in England and is part of the team offering the service to patients from across the largely rural county.
Hospital patients admitted with COVID-19 have been able to have anti-viral treatments in Lincolnshire since September 2021. These help boost a patient’s own immune system so that they are able to fight the virus sooner and prevent more serious symptoms and long term side effects.
Just before Christmas a new service was launched in the county, where patients diagnosed with COVID-19 who have underlying health conditions that mean that are at an increased risk of being admitted to hospital, can now have the anti-viral treatment as an outpatient.
They are referred to their service by their GP or NHS111, assessed by a nurse and a consultant to see if they are suitable for the treatment and then invited to attend an appointment at Lincoln County Hospital. They are then put on a drip and the anti-viral is delivered straight into their blood stream so that it can start working straight away. If they are assessed and unable to have the anti-viral intravenously, they may be offered an anti-viral tablet.
The Trust’s Medical Director, Dr Colin Farquharson, said: “In the first month more than 130 patients from across the whole of Lincolnshire have benefitted from this new outpatient service. The aim is to get these patients the treatment they need as soon as possible to prevent them from becoming seriously unwell from COVID-19. The feedback has been so positive and is testament to the hard work of everyone involved in helping to set up and run the service. It is very much a team effort that sees colleagues from across the Trust working with GPs, Lincolnshire Community Health Services NHS Trust and other healthcare partners from across the county.”
 Des Davis owns Margaret’s Tea Rooms in Lincoln and believes the team saved his life. Des, 54, has a condition that means he has a compromised immune system.
Des Davis owns Margaret’s Tea Rooms in Lincoln and believes the team saved his life. Des, 54, has a condition that means he has a compromised immune system.
He said: “I had started to feel unwell and it got a lot worse, very quickly. I did a lateral flow and also a PCR test and less than 24 hours later I knew I had COVID. By this time my symptoms were a lot worse and I was really starting to worry.
“When I got the call about the treatment I was so relieved. I went straight to the hospital, had the treatment and went home to bed.
“I still felt really poorly, at one point I kept getting sharp stabbing pains all over and I feared the worst, but gradually the symptoms started to wear off. I dread to think what might have happened if I hadn’t had the treatment. The team were all wonderful and I believe that they have saved my life. I will always be so thankful.”
Pictured below are members of the COVID Delivery Medical Unit team:
 |
Plymouth University launch National Dental Dementia Friendly Guide
The guide was produced by Professor Chris Tredwin Professor of Restorative Dentistry, Ian Sherriff B.E.M. Academic Partnership Lead for Dementia, Abby Nelder Community Engagement Programme Officer Peninsula Dental School, Claire Puckey BScHons and Tony Husband award-winning cartoonist. The guide was commissioned by the Prime Ministers National Dementia Challenge Group.
The guide enables all N.H.S dental practices in England to become inclusive Dementia Friendly Dentist in both rural and urban areas to create an enabling environment, engaging with people living with dementia, their families and carers. This makes it possible for people living with dementia to continue to have compassionate, individualised dental health care. A Dementia Friendly dental practice will enable people with dementia to have a sense of belonging and feel a valued part of a community and civic life. (Source: National Dementia Declaration 2012).
An inclusive Dementia Friendly dental practice works to sustain and improve the dental quality of life for people living with dementia which will reduce the impact of the lack of dental care, stigma, isolation and loneliness.
Dementia Friendly dental practices need to be flexible, adaptable and responsive to the different needs of people living with dementia and their carers. It is important to ensure that people living with dementia can continue to enjoy the previous dental support they had been receiving. The Guardian ran a full page on this project in their Dementia Health Sector (2021) As a result of this work Katy Kerr Associate Postgraduate Dental Dean Workforce Health Education England has invited Ian Sherriff B.E.M and professor Chris Tredwin to be part of a group working on a dental dementia learning programme(2022 and beyond).
Throughout 20219/21/22 the effects of COVID-19 have challenged all statutory and voluntary agencies working in rural communities to examine how they offer support and guidance to individuals living with dementia and their families. Local councils, as the most local form of government, have a major role to play in interpreting government and local COVID-19 plans to ensure that people living with dementia and their families continue to be included in all aspects of rural community life.
In response to the above challenges Ian Sherriff B.E.M University of Plymouth and Claire Goldfinch Policy Officer National Association of Local Councils (N.A.L.C) carried out a survey of all the 10,000 Parish and Town Councils in Rural England to gain an understand how they were supporting people living with dementia and their families. The overall response to this survey was “they wanted a Rural Dementia Parish and Town Councils Dementia Guide”. Armed with this response Ian Sherriff B.E.M and Claire Goldfinch (N.A.L.C) wrote a Rural Parish and Town Councils Dementia Guide (2020). The guide was sent to all the 10,000 Parish and Town Councils in England with a personal letter of support from the Prime Minister. Ian Sherriff B.E.M University of Plymouth and Silvia Elena Nicolé (N.A.L.C) will be sending out a follow up survey in February 2022 to establish how the Parish and Town Councils have implemented the recommendations in the Dementia Guide. This work was featured in the national and regional press.
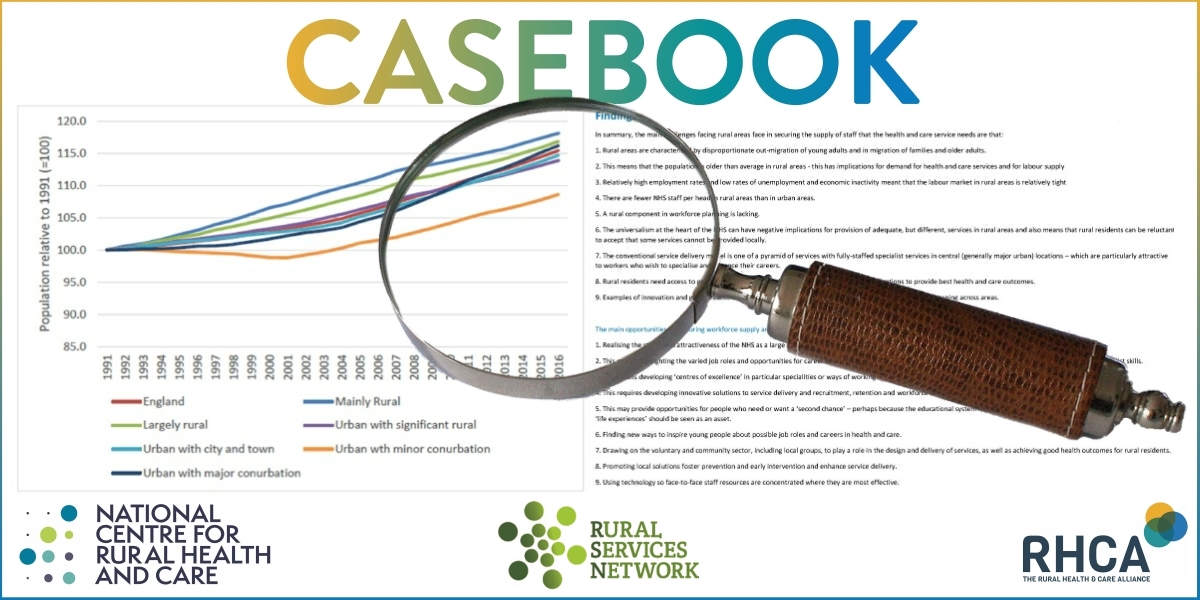
NATIONAL CENTRE UPDATE
Just one theme this month – our Parliamentary Inquiry Report on Rural Health and Social Care.
Parliamentary Inquiry Report
We were delighted to have approaching 150 virtual guests with the keynote provided by Sir Chris Whitty.
Here are some hyperlinks to different aspects of the coverage:
The Carer - UK • News • 1st February
Major Inquiry Highlights the Urban-Rural Divide in Accessing Health and Care
Today sees the launch of a major Inquiry into rural health and care. The three-year investigation undertaken by the All-Party Parliamentary Group (APPG) for Rural Health and Care and the National Centre for Rural Health and Care is one of the most extensive of its kind.
Social Care Today • News • 1st February
Major inquiry highlights the urban-rural divide in accessing health and care
Chaired by Anne Marie Morris, MP, the Inquiry was set up just prior to the Covid-19 pandemic to identify and ultimately address inequalities in rural health and care.
Localgov.co.uk • News • 1st February
Rural health services need 'levelling up', MPs say
A three-year investigation undertaken by the All-Party Parliamentary Group (APPG) for Rural Health and Care and the National Centre for Rural Health and Care has found stark levels of inequality between rural and urban areas when it comes to health and social care services.
Government Business • News • 1st February
Stark levels of health inequality between rural and urban areas
An investigation by the APPG for Rural Health and Care and the National Centre for Rural Health and Care has found stark levels of inequality between rural and urban areas when it comes to health and social care services.
We also achieved exposure on BBC Farming Today.
A post event press release is set out in edit form below:
The Levelling Up White Paper follows hot on the heels of the Inquiry into Rural Health and Care, launched on 1st February. This highlighted the various significant problems experienced by many rural citizens in accessing health and social care services. The Inquiry Report also emphasised the many factors that contribute to these access problems, ranging from poor digital connectivity to lack lustre public transport services. The funding of health and care in rural areas, in addition to poor community infrastructure, is at the heart of healthcare disadvantage.
At the launch event Professor Sir Chris Whitty, The Chief Medical Officer for England commented
“The health challenges of rural areas are distinct from those of urban areas, and they've received much less attention than they should have. So, I'm extremely grateful to the authors of this report, and those who've promoted it after doing so”.
Commenting on the Levelling Up agenda, NCRHC Chair Professor Richard Parish said:
"Healthcare is often viewed somewhat inappropriately as a cost. In truth, health and wealth are indivisible. Poor health is undoubtedly a cost to society. However, good health is an economic asset, contributing to improved productivity and a more efficient economy. What is more, economic improvement is fundamental to better health. It is a virtuous circle. Better health contributes to economic improvement and in turn a more vibrant economy leads to improved health outcomes.’ It is a classic ‘win-win’ scenario. This point is recognised in the Levelling-Up White Paper which says “The UK Government’s goal is to tackle the stark disparities in health outcomes across the UK, ensuring people have the opportunity to live long, healthy lives wherever they live. Better health improves productivity and well-being”.
We look forward to seeing the promised ‘White Paper designed to tackle the core drivers of disparities in health outcomes’ which must be fully rural proofed reflecting the evidence in our Inquiry report”
Reaction to the Report
Described by international observers as the most comprehensive review of its kind, the three-year Inquiry into Rural Health and Care, published by the National Centre and the All-Party Parliamentary Group (APPG) at the beginning of February, has been received to widespread acclaim.
Matthew Taylor, Chief Executive of the NHS Confederation said:
“This report identifies what many health leaders continue to tell us about the additional pressures experienced by health and care services in rural parts of the country.
“Filling workforce shortages is a particularly significant challenge facing rural healthcare services, which at its worst can add to waiting times, limit the breadth of services available locally, and lead to some people having to travel further to seek treatment.
“While the introduction of statutory integrated care systems and the development of primary care networks will hopefully lead to improvements and allow healthcare planning to take place across bigger regions, there are still around 93,000 vacancies, which will take time and resource to fill. A detailed and fully costed workforce strategy is urgently needed.
“NHS leaders are committed to working together to tackle these challenges but if the Government is serious about levelling up the country, it cannot overlook the deep-rooted disparities between rural and urban healthcare provision and patient experience.”
Commenting on the Inquiry Overview, the director of policy and strategy at NHS Providers, Miriam Deakin said:
“We welcome this report, which highlights the importance of understanding the distinct needs of rural areas, and ensuring structural, operational and financial challenges are taken into account in regulatory frameworks.
“This report reflects the complexity and diversity of the communities the trust sector serves, with rural areas facing unique challenges and opportunities, and requiring unique solutions.
“Delivering care across geographically dispersed communities is challenging for trusts across all sectors: whether large acute hospitals with isolated sites serving rural communities, ambulance trusts with large distances to cover or community and mental health trusts with a number of smaller settings based in rural areas."
FUNDING OPPORTUNITIES
This month we focus on five funding streams:
- Tudor Trust – funding to address marginalisation
- Money Saving Expert Charity – support for people in ill health to manage money
- NIHR – Health and Social Care Delivery Research Programme
- Medical Research Council – Developmental pathway funding scheme
- Medical Research Council - Populations and systems medicine research
To find out more about each of these funds click here
Spread the word
If you know of other organisations that you think would benefit from joining the Rural Health & Care Alliance, please click here to email us and let us know.
RURAL SERVICES NETWORK
Up to date news on Health and Care
The Rural Services Network provides a useful source of themed news content and data. Check out the latest news on Health & Wellbeing and Vulnerability, where you’ll find articles on a diverse range of rural issues affecting rural communities. You might also find this research on Over 65 Population Projections useful too.
Latest from RSN Member Insights
RSN Member Insights is the place to discover the statistics that define communities within our membership. It is regularly updated with new analyses, and these will be highlighted in the 'What's New' section of the RSN's Weekly Rural Bulletin. The Rural Bulletin also provides a selection of the most rurally topical news items, so do subscribe and encourage your colleagues to subscribe to what is an invaluable weekly periodical.
To make a suggestion of data that would benefit you by being included in the Member Insights section, please email Dan Worth, our Research and Performance Analyst, at [email protected].
| The Rural Health & Care Alliance is a membership organisation administered by the Rural Services Network on behalf of the National Centre for Rural Health & Care. Explore the RHCA service below: |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |